Covid remote monitoring
Covid Remote Monitoring
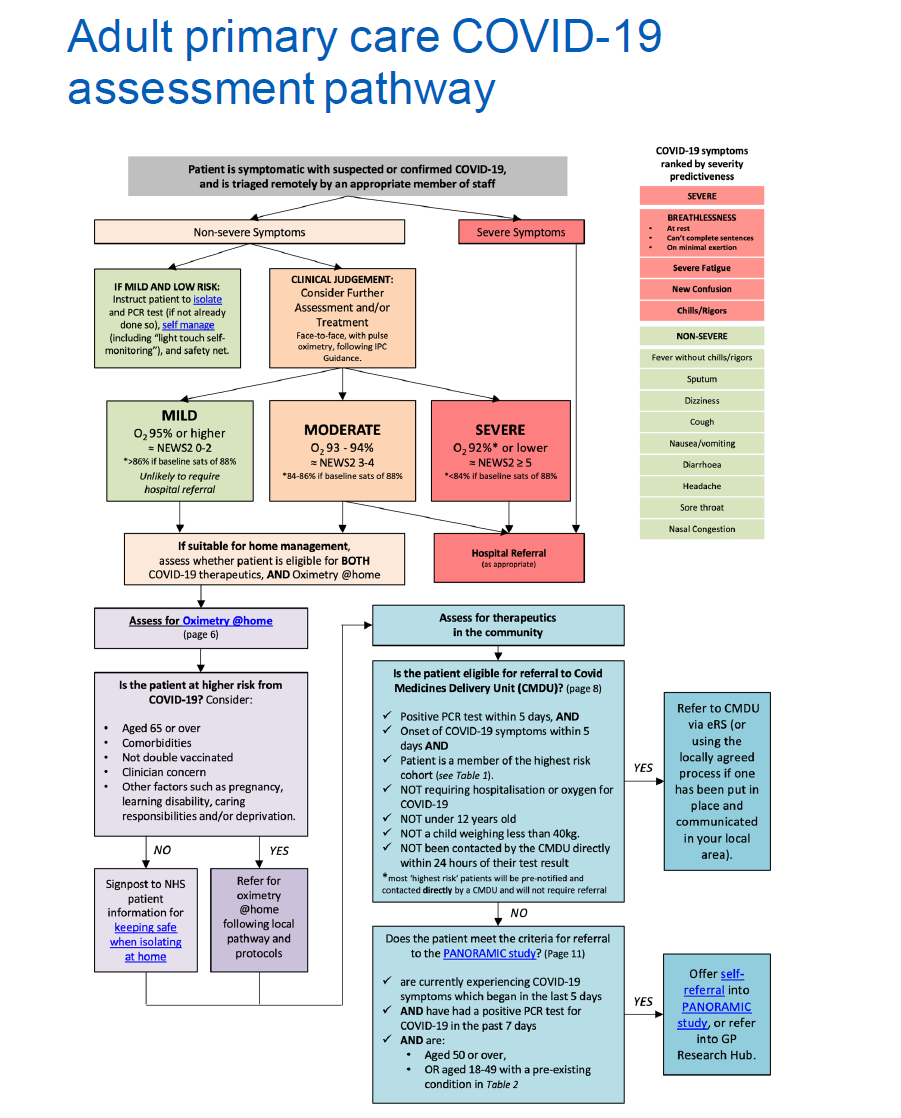
Delays in escalating patients’ care to hospital in the COVID-19 pandemic have resulted in patients being admitted to hospital with advanced COVID-19, thus requiring invasive treatment and potential admission to intensive care.
Remote home monitoring may help to reduce delays and identify at risk patients earlier.
Remote monitoring involves patient triage, providing patients with monitoring equipment, asking the patients to record their observations, monitoring calls from staff and follow-up once patients have been discharged from the service.
In November 2020, NHS England launched a national roll-out of this model of care called COVID Oximetry @ home.
In addition, in January 2021, NHS England launched a national roll out of early discharge models, referred to as ‘virtual wards’.
Covid@Home
What is Covid@Home/what is involved?
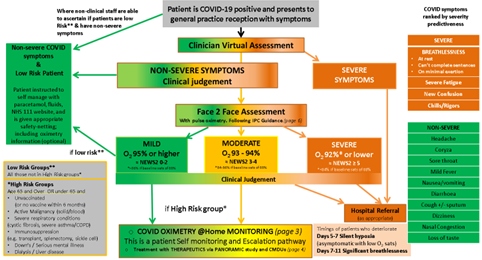
The use of oximetry to monitor and identify ‘silent hypoxia’ and rapid patient deterioration at home is recommended for patients most at risk of poor outcomes, who are best identified by oxygen levels.
Which patients are most at risk?
The type of monitoring a patient needs depends on their risk factors.
Risk factors include:
- Those aged 65 or over
- Co-morbidities
- Not double vaccinated
- Clinician concern
- Other factors, such as pregnancy, learning disabilities, caring responsibilities, deprivation
What is Covid@Home/what is involved?
The use of oximetry to monitor and identify ‘silent hypoxia’ and rapid patient deterioration at home is recommended for patients most at risk of poor outcomes, who are best identified by oxygen levels.
|
Self monitoring
|
Hub monitoring
|
Who Leads This Service?
This service is primary care (GP Practice) led.
Service Features:
With Covid@Home, the patient receives:
- A pulse oximeter and diary (paper or the HUMA app) to enable them to self-monitor 3 x a day
- Regular telephone calls and face-to-face or home visits, dependent on clinical need
The patient is monitored for up to 14 days depending on clinical need
For further information on using this service please refer to the Standard Operating Procedure
Covid Virtual Wards
What is a Covid Virtual Ward/what is involved?
Covid virtual wards aim to provide early and supported hospital discharge for patients with a primary diagnosis of COVID-19 who are referred from ED or have an improving clinical trajectory (symptoms, function, oxygen saturation) and have no fever for 24-48 hours consecutively (without medication to reduce fever).
Who Leads This Service?
Secondary Care - led by named Consultant or ST3+ with COVID experience.
Where is the service provided?
Within a patient’s home and acute trust
When and where is this service available?
Service available 7 days a week 08:00 – 20:00
May be integrated with 111/999 call handlers.
Service Features:
Patient receives
- Proactive daily calls (virtual ward round).
- A pulse oximeter and diary (paper or the HUMA app) to enable them to self-monitor 3 x a day
- Phone support line available during service hours (via a Healthcare support worker).
- Medication provided: e.g. O2.
The patient is monitored for up to 14 days depending on clinical need.
Cohorts that will benefit most from this service include
|
A diagnosis of COVID-19: either clinically or positive test result and being treated in secondary care services |
|
| X |
Patients with saturations greater than 93% low NEWS2 (< 3) and no desaturation or risks may be discharged to a Covid Virtual Ward where clinically appropriate (agreed by Senior Decision Maker) |
| X | Patients with saturations greater than 93% with improving clinical trajectories (symptoms, signs, blood results, CXRs), function can also be considered for Covid Virtual Ward |
Patients with oxygen saturations of 92% or lower or experiencing moderate/severe shortness of breath are generally unsuitable for early supported discharge, unless the patient is stable, and this is their usual baseline saturation.
Clinical judgement remains paramount for all assessments particularly for COVID patients with higher risk factors or other complicating medical conditions.
*Subject to completion of a satisfactory exercise test.
For further information on using this service please refer to the Standard Operating Procedure
Patient Assessment
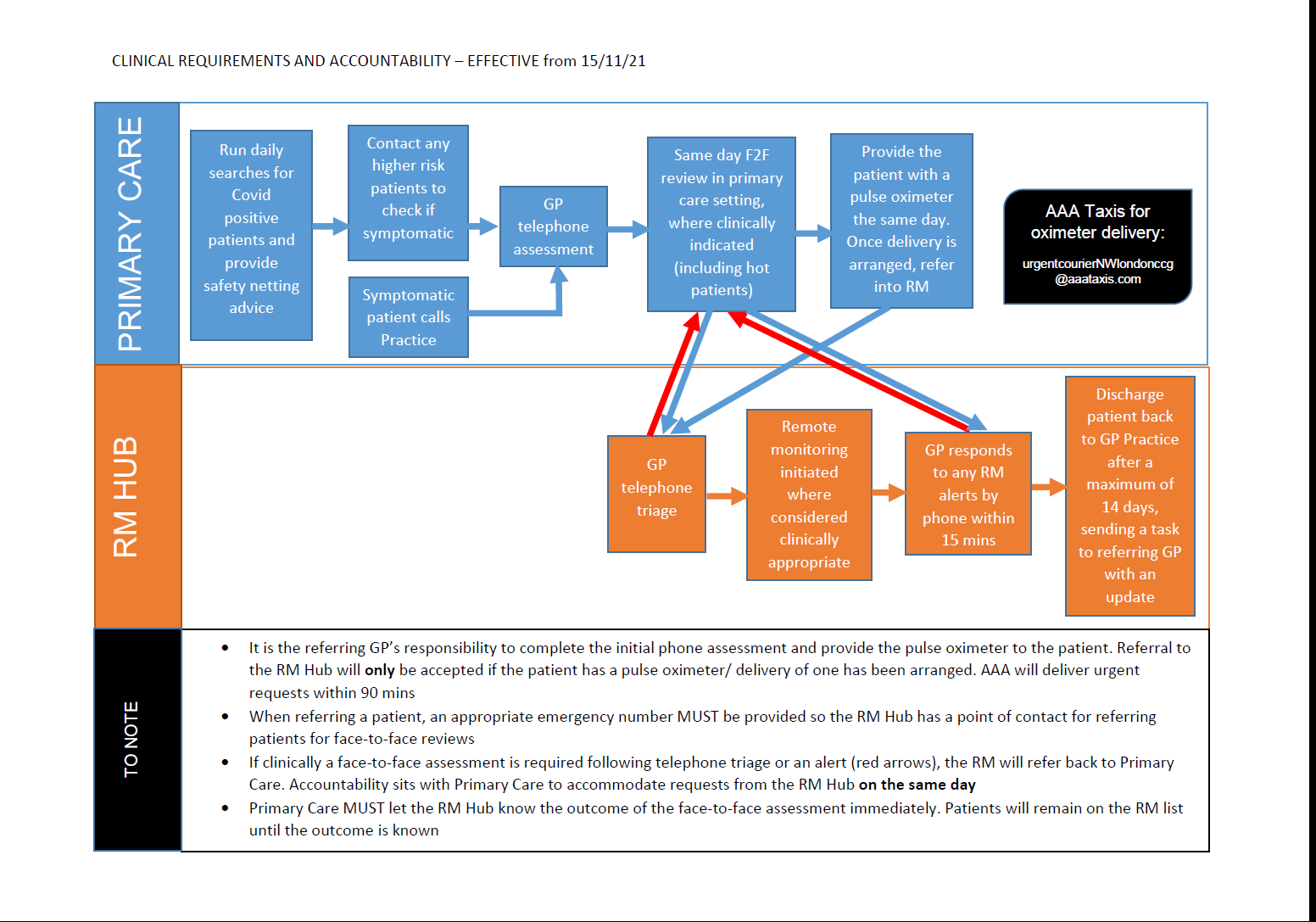
RM Hub Referral
Referral criteria:
Inclusion:
- Covid positive (PCR/LFT) or highly suspected and test result awaited AND
- Over 12 years AND
- Moderate symptoms AND high risk category
- High risk with mild symptoms can be self-monitored at home by GP practices
Exclusion:
- Patients who decline record sharing
- Covid negative
- Covid positive but mild symptoms or low risk
- No test done but mild symptoms or low risk – GP to tell them to get tested first
- Below 12 years of age
- >14 days of illness
- Patients for whom pulse oximeter delivery has not been organised
Pulse Oximeters
AAA Taxis provide a NW London-wide oxygen saturation probe loan service and will deliver to patients’ houses.
Oxygen saturation probes will be delivered to patients across London within 24 hours for routine requests and within 90 minutes for urgent requests
8am – 8pm/ 7 days a week (last urgent delivery at 6.30pm. Urgent referrals made after this time will be completed by 09.30am the following day)
BY CLINICIAN REQUEST AND WITH PATIENT CONSENT ONLY
Email: urgentcourierNWlondonccg@aaataxis.com
You must provide the following information:
- Confirmation that the patient has given consent to share their address details
- The name of the Hot Hub/Practice
- Your name
- The patient’s contact details (first name, address and telephone number)
- Whether the delivery is routine or urgent
Referrers will receive a confirmation of their request and confirmation of the delivery
Any issues should be reported on 01707 333666 (available 24/7)
Webinars
The NWL webinar, held on 4th February 2021, on Covid@Home and Covid Virtual Wards can be accessed via:
https://vimeo.com/510627905 (Password = NHS)
NWL GP Covid Update Webinar
Held on 12th January 2022, it can be accessed via:
NWL GP Covid Update Follow-on Webinar
Held on
Resources and Standard Operating Procedures
Useful Resources
Standard Operating Procedure: Oximetry in Primary Care
This Standard Operating Procedure (SOP) covers the process for the management of Covid Oximetry@home in general practice.
Standard Operating Procedure: NWL- Covid-19 Escalated Care Clinic
This Standard Operating Procedure (SOP) covers the process for the management of Covid Oximetry@home in Escalated Care Clinics.
Summary of Covid@Home and Covid Virtual Ward Pathways
This document focuses on Covid@Home and Covid Virtual Ward and aims to
provide a summary of the services, how they interrelate and how they differ.
This leaflet is for patients with suspected coronavirus who have not been admitted to hospital and will be isolating at home.
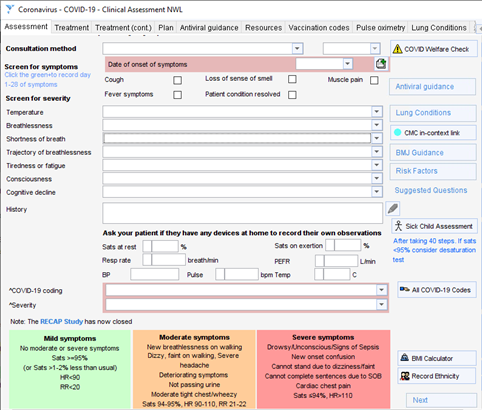
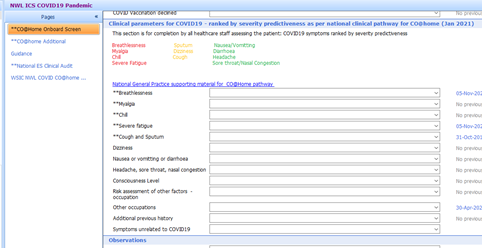
Oximetry@Home Templates On EMIS and SystmOne
This document provides a screen-shot/summary of the Oximetry@Home Templates On EMIS and SystmOne, which is designed to assit GPs in NWL to identify those patients at risk of deterioration from Covid-19 and enable early on-boarding into a Covid19 Oximetry@home service.
AAA Taxis Leaflet for Clinicians
Guide on how to carry out referral for oxygen saturation probe.
Practical tips on how to deliver an Oxygen@home service to your patients
Central London’s Covid-19 Guide for Practices
A summary guide for patients with Covid-19
Assessment, monitoring and management guide, NHS England
Guidance to support frontline clinicians with the assessment, monitoring and treatment of patients who present to general practice with symptomatic COVID-19.
SOP: Escalation Care Clinics – Extracting and Submitting Data
This document provides an overview of Extracting and Submitting Data from Escalated Care Clinics using SystmOne.
Letter from NHS England providing update on the UK four nations policy for providing neutralising monoclonal antibodies (nMABs) orantiviral treatments for the highest risk non-hospitalised patients for 12 years and over with COVID-19.








